Infrared light therapy (ILT) is a non-invasive treatment that uses infrared light to promote healing, reduce pain, and improve overall health. This therapy harnesses the benefits of infrared wavelengths, which penetrate the skin and stimulate biological processes that enhance physical well-being. The therapeutic effects of infrared light have been explored in various medical fields, making ILT a popular option for individuals seeking alternative or complementary treatments for a range of conditions.
Definition
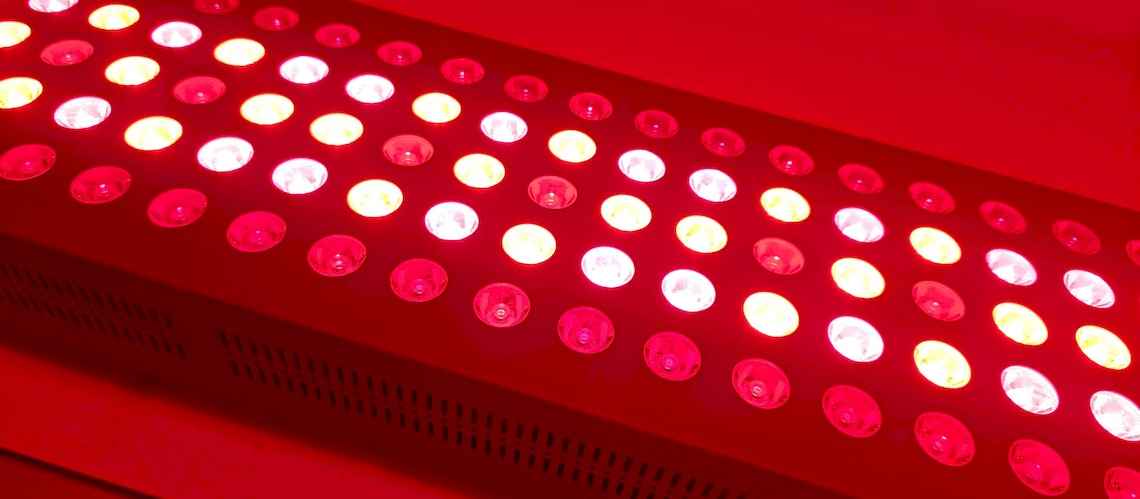
Infrared light therapy involves the application of infrared light, typically emitted by devices such as LEDs or infrared lamps, to deliver energy to the body’s cells. This energy absorption at the cellular level enhances mitochondrial function, promoting healing processes and cellular regeneration. Research has shown that ILT can effectively treat a variety of health conditions, making it a versatile therapeutic modality (Hamblin, 2017).
History and Origins
The use of light for therapeutic purposes dates back to ancient civilizations, such as the Greeks and Egyptians, who used sunlight to treat various ailments (McDonagh, 2001). Modern infrared light therapy, however, emerged in the mid-20th century, spurred by advancements in light technology. Notably, NASA’s research into the effects of infrared light on plant growth in space environments revealed its potential for human health applications. This discovery led to extensive studies on the benefits of infrared light for promoting tissue repair and reducing pain in astronauts and subsequently in clinical settings on Earth (Whelan et al., 2003).
Principles and Concepts
Photobiomodulation
The primary mechanism of ILT is photobiomodulation, a process where light energy is absorbed by cellular mitochondria. This absorption increases the production of adenosine triphosphate (ATP), the cell’s energy currency, enhancing cellular repair, regeneration, and overall function (Hamblin & Demidova, 2006). The increased ATP production is associated with reduced oxidative stress and inflammation, contributing to the therapeutic effects observed in various conditions (Hamblin, 2017).
Penetration Depth
Infrared light has a longer wavelength than visible light, allowing it to penetrate deeper into tissues. Studies have shown that infrared light can reach depths of up to several centimeters, making it particularly effective for treating deep-seated pain, inflammation, and musculoskeletal conditions (Chung et al., 2012).
Benefits
Infrared light therapy offers numerous scientifically supported health benefits, including:
- Reduced Inflammation and Pain: ILT has been shown to decrease inflammatory markers and reduce pain in various conditions, such as osteoarthritis and chronic lower back pain (Baroni et al., 2010; Chow et al., 2009).
- Enhanced Wound Healing and Tissue Repair: The therapy promotes wound healing by accelerating collagen production and cellular repair mechanisms (Posten et al., 2005).
- Improved Circulation: Infrared light has vasodilatory effects, improving blood flow and oxygen delivery to tissues, which aids in healing and recovery processes (Chung et al., 2012).
- Relief from Chronic Pain Conditions: ILT is effective in managing chronic pain conditions, such as fibromyalgia, by modulating pain perception and reducing inflammation (Chow et al., 2009).
- Enhanced Muscle Recovery and Performance: Athletes have reported faster recovery times and improved performance following ILT, supported by studies showing reduced muscle soreness and enhanced muscle repair post-exercise (Leal-Junior et al., 2015).
Applications
Infrared light therapy is utilized in various medical and wellness settings, including:
- Pain Management Clinics: ILT is frequently used to manage chronic pain, with evidence supporting its efficacy in conditions like arthritis and neuropathic pain (Hamblin, 2017).
- Physical Therapy Centers: Therapists incorporate ILT into rehabilitation programs to enhance recovery from injuries and surgeries by improving tissue healing and reducing inflammation (Chung et al., 2012).
- Sports Medicine Facilities: Athletes use ILT to accelerate muscle recovery and reduce the risk of injury, supported by research demonstrating its benefits for muscle performance and recovery (Leal-Junior et al., 2015).
- Home Wellness Devices: Portable ILT devices have become popular for personal use, allowing individuals to manage pain and promote healing in the comfort of their homes (Hamblin, 2017).
For consumers seeking to replicate the benefits of infrared light therapy at home, LED-based devices present a practical and scientifically supported option for many therapeutic purposes. Studies show that LED therapy can promote healing, reduce inflammation, and alleviate pain when applied at the appropriate wavelengths (600–1000 nm), similar to those used in Low-Level Laser Therapy (LLLT) (Chung et al., 2012). While LLLT utilizes coherent laser light, research indicates that the scattering and absorption properties of human tissue cause both laser and LED light to become diffuse upon contact, minimizing differences in their effects for superficial and moderate-depth applications (Chung et al., 2012; Leal-Junior et al., 2015). LED devices for home use are designed to deliver energy densities within the therapeutic range, making them an effective and accessible choice for general recovery and wellness. However, LLLT may retain advantages for conditions requiring deeper tissue penetration or specialized treatment, and individuals with specific medical concerns are advised to seek professional guidance to ensure optimal results (Ruh et al., 2018).
Scientific Evidence
Extensive research highlights the efficacy of infrared light therapy in reducing inflammation, promoting healing, and alleviating pain. For example, a study published in Lasers in Surgery and Medicine demonstrated significant improvements in chronic lower back pain, with reduced pain levels and improved functionality (Chow et al., 2009). Similarly, research in Lasers in Medical Science found that low-level laser therapy enhanced wound healing in diabetic patients by promoting tissue growth and improving the balance of key repair-related markers in the body (Ruh et al., 2018). However, it is important to note that studies comparing LED therapy and LLLT for deeper tissue applications remain limited, and further research is needed.
How to Get Started
Consultation
Before starting ILT, consult with a healthcare provider to determine its suitability for your specific health needs. This step is crucial, especially for individuals with underlying medical conditions or those on medications that may be affected by light therapy (Hamblin, 2017).
Devices
Choose a reputable infrared light therapy device, such as an LED panel or infrared lamp, ensuring it meets safety and efficacy standards. Look for devices that offer appropriate wavelengths (typically 700–1000 nm) for therapeutic use (Hamblin, 2017).
Application
Follow the recommended usage guidelines, typically involving daily sessions of 10–20 minutes. Consistency is key to achieving optimal results, and it is important to use the device as directed to avoid potential side effects, such as skin irritation (Hamblin, 2017).
Case Studies or Testimonials
Numerous case studies and testimonials support the benefits of ILT. For instance, athletes have reported faster muscle recovery and reduced injury downtime, supported by research on photobiomodulation’s effects on muscle performance (Leal-Junior et al., 2015). Similarly, individuals with chronic pain conditions, such as fibromyalgia, have found significant relief through consistent use of ILT, as evidenced by clinical studies and patient testimonials (Chow et al., 2009).
Conclusion
Infrared light therapy offers significant potential for enhancing physical health and well-being through scientifically validated mechanisms. By harnessing its benefits, individuals can achieve reduced pain, accelerated healing, and improved overall vitality. As ongoing research continues to expand our understanding of its applications, ILT holds promise for non-invasive, accessible treatments in medical and wellness contexts. Consumers are encouraged to explore reputable devices and consult professionals to ensure safety and maximize results.
References
- Baroni, B.M., Leal Junior, E.C.P., De Marchi, T., Lopes, A.L., and Salvador, M. (2010) ‘Low-level laser therapy before eccentric exercise reduces muscle damage markers in humans’, European Journal of Applied Physiology, 110(4), pp. 789–796.
- Chow, R.T., Johnson, M.I., Lopes-Martins, R.A., and Bjordal, J.M. (2009) ‘Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials’, Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. Centre for Reviews and Dissemination (UK). Available at: https://www.ncbi.nlm.nih.gov/books/NBK78464/.
- Chung, H., Dai, T., Sharma, S.K., Huang, Y.-Y., Carroll, J.D., and Hamblin, M.R. (2012) ‘The nuts and bolts of low-level laser (light) therapy’, Annals of Biomedical Engineering, 40(2), pp. 516–533.
- Cotler, H.B., Chow, R.T., Hamblin, M.R., and Carroll, J. (2015) ‘The use of low-level laser therapy (LLLT) for musculoskeletal pain’, MOJ Orthopedics & Rheumatology, 2(5), p. 00068.
- Hamblin, M.R., and Demidova, T.N. (2006) ‘Mechanisms of low-level light therapy’, Proceedings of SPIE, 6140, pp. 1–12.
- Hamblin, M.R. (2016) ‘Shining light on the head: photobiomodulation for brain disorders’, BBA Clinical, 6, pp. 113–124.
- Hamblin, M.R. (2017) ‘Mechanisms and applications of the anti-inflammatory effects of photobiomodulation’, AIMS Biophysics, 4(3), pp. 337–361.
- Leal-Junior, E.C.P., Lopes-Martins, R.A., and Bjordal, J.M. (2015) ‘Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis’, Lasers in Medical Science, 30(2), pp. 925–939.
- McDonagh, A.F. (2001) ‘Phototherapy: From Ancient Egypt to the New Millennium’, Journal of Perinatology, 21(S1), pp. S7–S12.
- Posten, W., Wrone, D.A., Dover, J.S., Arndt, K.A., Silapunt, S., and Alam, M. (2005) ‘Low-level laser therapy for wound healing: mechanism and efficacy’, Dermatologic Surgery, 31(3), pp. 334–340.
- Ruh, A.C., Frade, M.A.C., Bagnato, V.S., and Kurachi, C. (2018) ‘Laser photobiomodulation in pressure ulcer healing of human diabetic patients: gene expression analysis of inflammatory biochemical markers’, Lasers in Medical Science, 33(1), pp. 165–171.
- Whelan, H.T., Smits, R.L., Buchmann, E.V., Whelan, N.T., Turner, S.G., Margolis, D.A., Cevenini, V., Stinson, H., Ignatius, R., Martin, T., and Cwiklinski, J. (2003) ‘Effect of NASA light-emitting diode irradiation on molecular changes for wound healing in diabetic mice’, Journal of Clinical Laser Medicine & Surgery, 21(2), pp. 67–74.